Evans discusses BWWMH future with Demopolis Rotary
Demopolis’ hospital will “take a ‘selfie’” over the next three months as it conducts a Community Health Needs Assessment (CHNA).
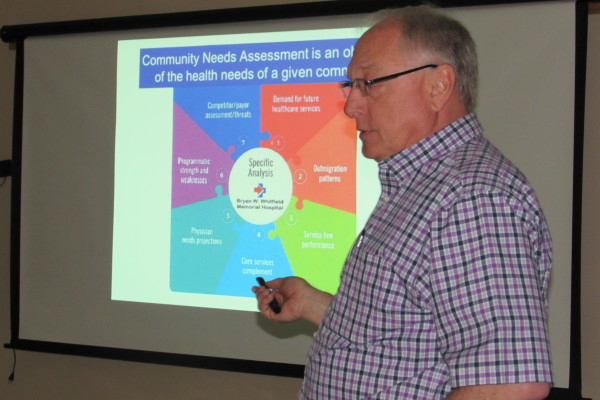
Art Evans, CEO/administrator of Bryan W. Whitfield Memorial Hospital, told members of the Rotary Club Wednesday the assessment, being conducted by an independent agency, will cover demand for future services, where patients go if not to the local hospital, service time performance, core services, physicians’ needs and a SWOT analysis.
The last such CHNA occurred five years ago, Evans said. They are conducted on a regular basis to gauge how well the hospital is doing and how it can improve.
Part of the CHNA will be a survey of stakeholders in the five-county area the hospital covers, he continued. People such as health care professionals, elected officials and community leaders will be asked to give their opinion on improving hospital services.
Once the CHNA is complete, the hospital must set out an implementation strategy to address improvement issues as mandated by the IRS. The assessment helps the hospital recognize trends so that it can be proactive in preparing for the future.
Evans also talked about the issue of Medicaid funding in Alabama. Medicaid, he said, is limited to children, pregnant women, the elderly and disabled. Alabama has the most restrictive eligibility standards in the country since those requesting aid cannot make more than $2,867 a year.
For every 32 cents the state puts into Medicaid, the federal government adds 68 cents. Alabama has the third lowest cost per enrollee in the country.
The proposed legislation to add only $15 million to the Medicaid budget will fall far short of what is needed, Evans continued. “Level funding is going to force Medicaid to cut services,” he said.
The hospitals and medical professionals in the state have been working for the past two years on a Regional Care Organization plan which would start Oct. 1. Because it is done within the state and each RCO would manage its allocated funds, the usual 15 percent administrative fee would not have to be paid to an outside insurance company to oversee, saving costs for the state.
However, unless more money is added to the Medicaid budget, the RCOs are in jeopardy of not being able to begin and help keep down health care costs for those in need.
Evans stressed to the Rotarians that hospitals in the state get no money from the General Fund Budget. Hospitals themselves pay into a state fund that is matched at the federal level three-to-one. That money is returned to the hospitals after the state takes out 15 percent for the Medicaid agency.
The General Fund Budget, he explained, helps pay for physicians, pharmacies and nursing homes.
To help generate more funds for the hospital, Evans said BWWMH is taking advantage of the federal influx of $750 million to help jump-start the RCO program by submitting plans on how to save money in the long run. If approved, the hospital will be rewarded monetarily.
The hospital, said Evans, expected to submit three plans on Thursday. They include a more efficient admittance of patients to the Emergency Department, whether there for clinical ailments or more critical needs; group physicians to handle more Medicaid patients, and better use of the Health Care on Wheels van.
The hospital has received a $900,000 grant to extend the Health Care on Wheels for one year. It will equip the van and physicians’ offices, including technology to connect the van to doctors’ offices, and will pay for the doctors, nurses and nurse practitioners to man the van.
The van started last week and will have a rotating two-week schedule through the rural areas of the five counties the hospital serves.
The hospital on Tuesday received its audit report. While the auditors gave it a clean report, Evans said it showed that operating costs are 107 percent of the net patient service revenue.
The good news, he said, is that it is the lowest cost-to-revenue among the peer hospitals that the auditors used as comparisons.
Hospitals now have to rely on other sources of revenue besides patients paying their fee. The difference between BWWMH and the other hospitals it was compared to is that the others received millions of dollars in local government support.
The local hospital lost $650,000 in 2015. Thanks to cost-cutting measures and more efficient operations, the loss is considerably less that previous years. It is trending in the right direction, said Evans.

